PERH (The North Estonia Medical Centre) is one of the top healthcare providers and larger hospitals in Estonia.
The project was set in motion as an international collaboration involving the Estonian Connected Health Cluster, Government Office of Estonia, North Estonia Medical Centre, Estonian Academy of Arts, University of Lapland, Lapland Central Hospital, University of Gothenburg, Academy of Design and Crafts, Sahlgrenska School of Innovation and Entrepreneurship, and Sahlgrenska University Hospital.
Project length
4 months
Collaborators
Maria Del Mar Salazar Soto
Triin Jürgens
Mentors
Ionel Lehari
Ruth-Helene Melioranski
Healthcare in transition
Healthcare systems in Estonia are in transition — currently towards a quantitive systematic approach. As new discoveries and technological advances raise the quality and opportunities in healthcare, more and more people become eligible for treatments where previously medicine was unequipped to provide relief. This has called for raise in efficiency which in turn has distanced the system from a personal approach towards the patients. Holding no negative or positive connotation on its own, it merely calls for a shift in approach — an opportunity to be seized.
The relationships between the different parts of the hospital system are complex. In our process we set to understand the interconnectivity and dependency of all parts. Instead of looking from a viewpoint of a particular actor, we made use of various viewpoints in order to make observations that hold stronger ground. In the context of PERH, a co-designing approach allows for combining multiple perspectives and in that for a richer, more holistic picture of the existing complexities.
Finding the focus
During the initial information gathering we were introduced to PERH and given a tour of the clinics. In our team of three students, we decided to focus on the day surgery clinic.
PERH Day surgery clinic is fascinating as it operates differently from other clinics of the same hospital. In a way it can be viewed as a facility for surgeries — patients come in for surgical procedures that are performed by corresponding surgeons of the hospitals. The main requirement for surgery to be eligible for the clinic is that the patient can leave the hospital on the evening of the surgery.
After a thorough tour of the clinic, we had a good overview to form our general understanding of the clinic and make first assessments on what to focus on in the interview process.
Stakeholder interviews
In order to understand the different experiences and expectations of all actors involved we organised and conducted 17 interviews with patients, surgeons, nurses, the head of surgery, the head nurse, the secretary of the clinic, the head of customer service and others.
Since hospital staff are very busy, we had to be flexible with planning our interviews, having even interviewed a surgeon while he was operating on a patient. Gathering information in such high intensity situations gave us insight we wouldn’t have gained otherwise.
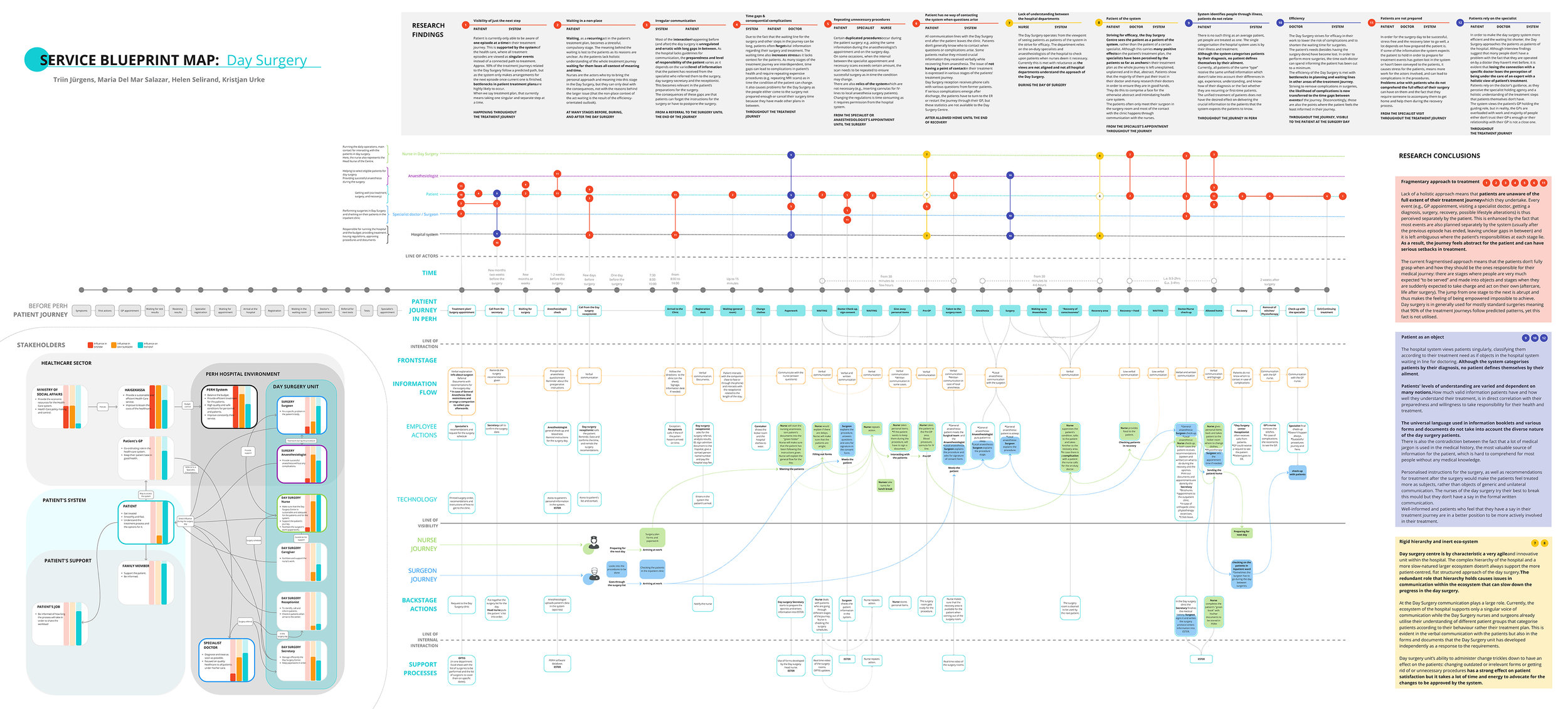
Mapping out the complexity
When the system is as complex as the one in PERH the necessity for maps presents itself. The level of complexity becomes so high that without one, information and connections can start slipping. Mapping all the interviews in a complex mindmap allowed me to compare the viewpoints of different actors and perceive that to all actors the system is very different. There is no single problem patient or a single problem for that matter, there is no well-behaving patient, it is rather a matter of perception and a matter of communication. Comparing side-by-side what actors were saying opened the system in its full complexity. Mapping the journeys allowed to always understand what moments different actors were talking about and to see all the actors in motion in these moments. Mapping out the stakeholders and their levels of influence gave more understanding to their actions.
The maps allowed me to see the holistic picture of how the findings form and how they connect, how parts of the system form a whole. This is especially important as we are dealing with a unit in the system that currently is facing difficulties fitting into the larger ecosystem. The relations between the encompassing unit and the smaller unit contained within form the basis of any future development and design implementation dealing with a more holistic approach.
Findings as the foundation of the design phase
The key insight from our research shows that patients’ treatment plans currently are managed fragmentarily, leading to every event (e.g. GP appointment, specialist appointment, waiting list, surgery, recovery, possible lifestyle alterations) being perceived separately also by the patient. When treatment events are planned separately by the system (usually after the previous episode has ended), it leaves unnecessary gaps in time in between and in consequence it becomes ambiguous where the patient’s responsibilities at each stage lie. As a result, the journey becomes abstract for the patient and thus can have serious setbacks in treatment.
There is an opportunity to support a more holistic approach towards the whole treatment plan of a patient and in that allow for the patient to be more informed, empowered, prepared, and responsible in their own healthcare. This would allow for the patients to be better equipped to be involved in making the decisions about their treatment options and becoming more engaged in the treatment plan resulting in reduced complications and in improved health.
An intense week of
co-design
In the ideation phase we worked closely together with experts from various related fields. During a week-long intense phase on the hospital premises our team met with actors from the Day Surgery department on various occasions, along with hospital management, the IT department, physiotherapists, ministry experts and service designers with previous experience in similar projects.
Within that week we developed our main concept idea and got direct feedback to it from the hospital actors and experts in order to take the next steps to develop the idea further and finalise our design concept.
Introducing Amicus
Every industry has a human element, but human connection is the heart of medicine.
Trust towards doctors and nurses is often the primary driver of patient behaviour. Patients are more likely to open up and share information, but also follow treatment plans, if they trust their healthcare specialist. Better quality of interaction results in greater patient autonomy and shared decision-making.
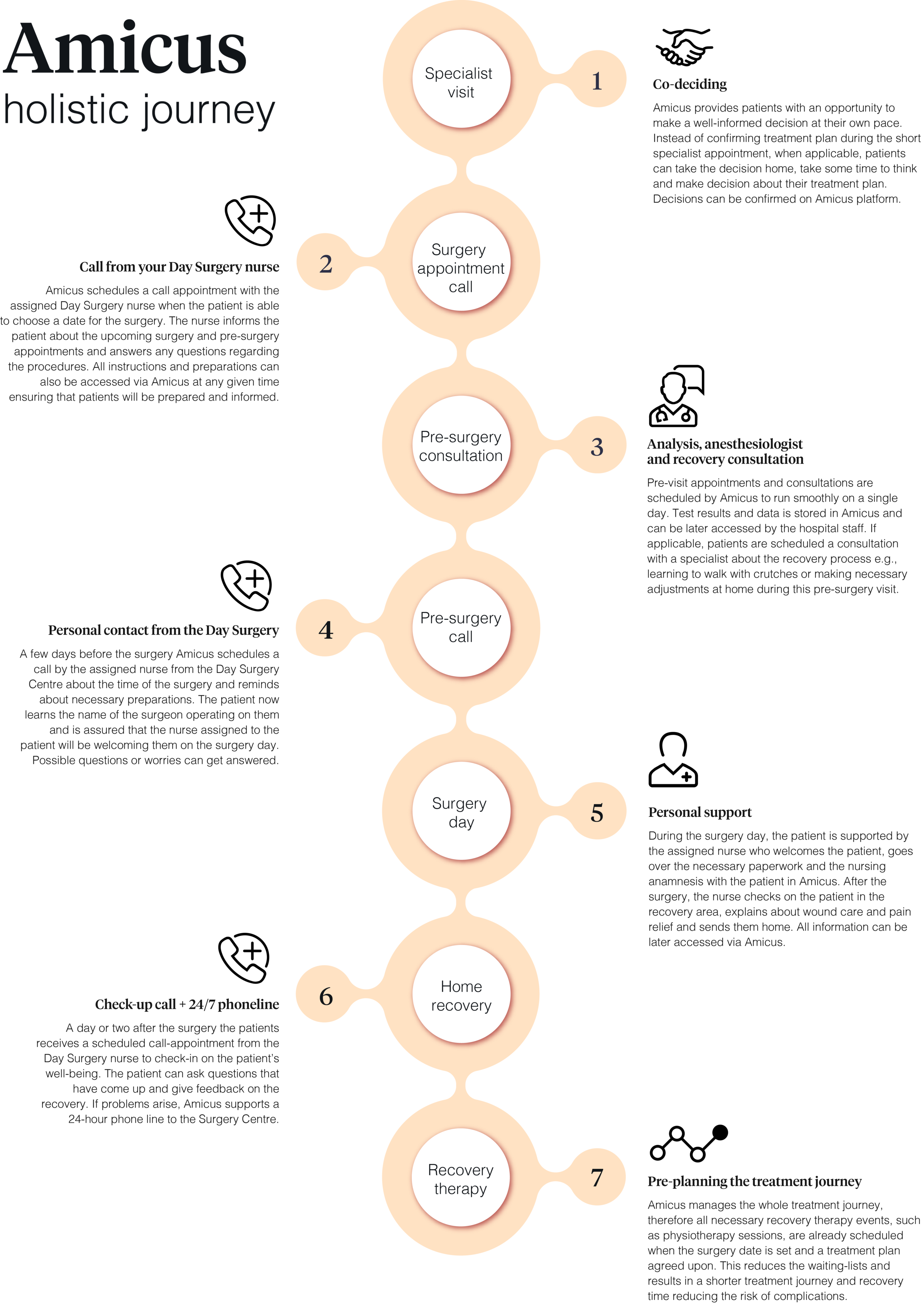
Amicus brings forward the nurse as the main point of contact
Nurses are highly educated and equipped medical personnel who, with the help of Amicus, are able to follow the patients’ whole treatment journeys and answer any questions the patients may have about it. This is not a big leap at all from what they are already managing today.
Having a friendly voice and face supporting the patients during their journey adds trust for the patients. Amicus allows patients to be under the care of a dedicated nurse during their treatment journey who would also be the one to call the patient to inform them about their surgery time, welcome them on the day of the surgery and make a call appointment a day or two after the surgery to check on the patient and answer any remaining questions.
Amicus gathers and manages all schedules and resources
This means that surgery lists, appointments, and staff schedules don’t have to be put together manually – this kind of work is time-consuming and prone to human error. Automation of these processes results in higher reliability, availability, and reduced costs.
More importantly, it frees up human resources which means there is more time for person-to-person interaction with patients for the assigned nurses.
With Amicus hospital staff can check their schedules and surgeries and patients can access their treatment journeys. Nurses are able to look at their daily schedules including their assigned patients as well as call appointments and start filling out the documentation for the surgery patients.
In a way, Amicus acts as a bridge between the hospital and patients, allowing them to communicate with one another more freely, reducing the unnecessary and allowing to focus on what really needs to be communicated.
Being able to make choices about one’s health is the key towards more engaged individuals and a more health-conscious society.
Amicus enables patients to actively participate in decision-making. Whenever possible, giving them an opportunity to decide over treatment options or simply give them time and have a moment to think it over before acknowledging an upcoming surgery. Even having a say about a surgery date is a step towards more active involvement.
An important feature of Amicus is a clear understanding and visibility of the treatment journey.
Patients can access information about their treatment throughout their treatment journey and zoom into each step. The system reminds patients about upcoming events through notifications and helps to keep track of each stage of the treatment journey.
Technical advancements can and should foster progress but technology alone means little without the human connection between patients, doctors and nurses. But when designed well, what technology can do is enable a stronger bond through increased personalised communication and understanding, and help to create a more patient-centred experience.
Amicus strengthens human connection and trust in healthcare by combining personal interaction with system automation.
Amicus supports a holistic treatment journey and hospital schedule management powered by an intelligent algorithm. With Amicus patients have an assigned nurse as a single contact person, can follow and access information on the go and be actively involved in every step of their treatment journey.
Amicus provides doctors, nurses, and administrators with valuable data but also allows patients to feel cared for, even at a distance, so that patients become involved in their own health.
After the project concluded…
Amicus was developed as a design concept and handed over to the Day Surgery department of PERH. Although the project itself concluded and the budget to fully develop the concept has not been allocated, the hospital has taken steps to implement ideas Amicus brought to attention. Currently, the Day Surgery department and the IT department are working on solutions how to notify patients more conveniently about upcoming appointments. A physiotherapist has been brought in to consult the patients about their recovery at home and the necessary precautions in their treatment before surgery time.
It was a successful collaboration project and in many ways we owe it to the incredibly supportive, cooperative, and accommodative staff of the Day Surgery of the North Estonia Medical Centre.